WHO issues urgent guidance to help countries confront global health financing crisis
Geneva, Switzerland (3 November 2025) – The World Health Organization (WHO) has released a new set of recommendations to help countries address the devastating impact of sudden and severe cuts in external health funding, which are threatening the continuity of essential health services across low- and middle-income nations.

The guidance, titled “Responding to the health financing emergency: immediate measures and longer-term shifts,” outlines both short-term and structural solutions to help governments withstand financial shocks and build sustainable, self-reliant health systems for the future.
Health funding cuts threaten essential services
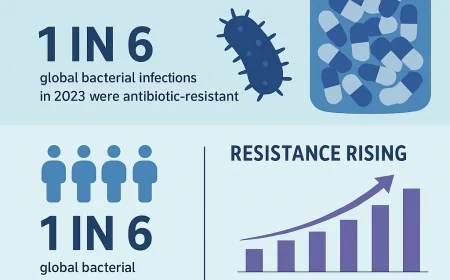
According to WHO data, external health aid is projected to fall by 30–40% in 2025 compared to 2023, resulting in immediate disruptions to vital health programs. Survey results from 108 low- and middle-income countries (LMICs) collected in March 2025 show reductions of up to 70% in critical services such as maternal and child care, vaccinations, health emergency preparedness, and disease surveillance.
More than 50 countries have reported job losses among health and care workers, as well as interruptions in training programs — threatening years of progress toward universal health coverage.
“Sudden and unplanned cuts to aid have hit many countries hard, costing lives and jeopardizing hard-won health gains,” said Dr. Tedros Adhanom Ghebreyesus, WHO Director-General. “But this crisis also presents an opportunity to shift from dependency on external aid to sustainable domestic financing that ensures health systems can stand on their own.”
Policy priorities for resilience and equity
The WHO guidance urges national governments to treat health spending as a strategic investment in social and economic stability, not merely a budgetary cost. It calls on policymakers to take swift, evidence-based action guided by principles of efficiency, equity, and sustainability.
Key recommendations include:
-
Prioritizing health services for the poorest and most vulnerable populations.
-
Protecting health budgets and maintaining essential service delivery even during fiscal crises.
-
Improving efficiency through better procurement systems, reduced administrative overhead, and strategic purchasing.
-
Integrating donor-funded programs into comprehensive, primary health care (PHC) delivery models.
-
Using health technology assessments to identify high-impact interventions with the best value for money.
Country responses show leadership amid crisis
Several nations have already taken decisive action to reinforce their health systems despite declining foreign aid.
-
Nigeria increased its national health budget by US$200 million to offset aid shortfalls, expanding funding for immunization, epidemic response, and key health programs.
-
Ghana removed the cap on excise tax earmarked for its National Health Insurance Agency, boosting its budget by 60% and launching The Accra Reset — a framework to reform global health governance and financing.
-
Kenya and South Africa have proposed budget increases for health pending parliamentary approval.
-
Uganda is implementing an integration policy for health services to improve efficiency and maintain long-term sustainability.
WHO and partners strengthen global cooperation
The new guidance aligns with the World Health Assembly’s resolutions on “Strengthening health financing globally” and “Economics of health for all.” It reinforces WHO’s mission to help countries achieve universal health coverage (UHC) through resilient, equitable, and efficient systems.
To support implementation, WHO is launching the UHC Knowledge Hub in partnership with the Government of Japan and the World Bank in December 2025. The hub will provide technical expertise, data analytics, and peer learning to help countries navigate the transition toward sustainable health financing.
“Global solidarity and national leadership must go hand in hand,” said Dr. Tedros. “With sound policy and cooperation, countries can safeguard essential services today while building stronger, fairer, and more resilient health systems for tomorrow.”