AI tool could cut failed organ transplant attempts by 60 per cent
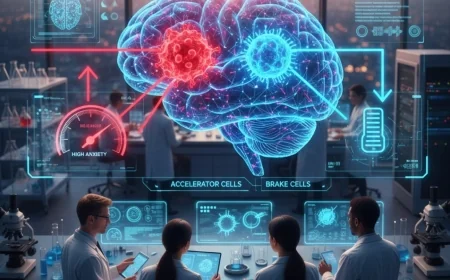
Researchers at Stanford University have unveiled an Artificial Intelligence (AI) tool designed to significantly reduce the number of failed liver transplant attempts by accurately predicting organ donor viability. The machine learning model forecasts whether a donor will die within the critical time window that preserves organ quality, a task that currently relies heavily on human judgment.

The new tool could potentially cut futile procurements—when surgery preparations begin but the organ becomes unusable—by 60%, compared with predictions made by experienced surgeons.
Addressing the DCD Challenge
The AI tool addresses a major challenge in Donation after Circulatory Death (DCD), where a donor dies after cardiac arrest following life-support withdrawal. In DCD liver transplants, the time between life support removal and death must not exceed approximately 45 minutes. If the donor survives too long, the organ quality deteriorates due to lack of oxygen (ischemic injury), forcing surgeons to reject the liver and increasing risks for recipients.
Currently, about half of DCD procedures are canceled due to this time-critical challenge.
Dr. Kazunari Sasaki, clinical professor of abdominal transplantation and senior author on the study, noted that the model could identify the likelihood of an organ being useful before any surgery preparations begin, making the transplant process more efficient.
How the Model Works
The Stanford-led model was built and trained using neurological, respiratory, and circulatory data from more than 2,000 donors across multiple US transplant centers.
-
The system uses pattern recognition across multiple physiological signals to track the progression toward death in a way that human observers may miss.
-
The model maintained accuracy even when some donor information was missing.
-
In testing, the AI consistently outperformed human predictions, accurately predicting the donor’s time of death 75% of the time, compared to surgeons' average accuracy of 65%.
The researchers believe this data-driven approach shows "the potential for advanced AI techniques to optimise organ utilisation from DCD donors" and could help teams decide which donors to pursue, potentially increasing the successful transplant rate and reducing the considerable costs associated with canceled procedures. The team plans to adapt the model for heart and lung transplants next.